What Type of Mutation Causes Sickle Cell Disease: The Role of Genetic Mutations
Wondering what type of mutation causes sickle cell disease? You’ll find the answer in this article. Sickle cell disease (SCD) is a genetic disorder where abnormal hemoglobin molecules in red blood cells.
This leads to various complications. These can be chronic pain, organ damage, and increased infection susceptibility.
If you wonder is RSV contagious? A connection exists between respiratory syncytial virus, causing infections in children with sickle cell disease.
This debilitating condition affects millions of people worldwide, particularly those of African, Mediterranean, Middle Eastern, and South Asian descent.
The symptoms of sickle cell disease are known to be:
- Episodes of pain,
- Anemia,
- Frequent infections,
- Swelling of feet and hands,
- Vision problems,
- Delay in puberty or growth
In this informative article, we’ll explore the genetic mutations responsible for sickle cell disease. Including their underlying mechanisms, and the impact of this disorder on individuals and communities.
Contents
Genetic Basis of Sickle Cell Disease
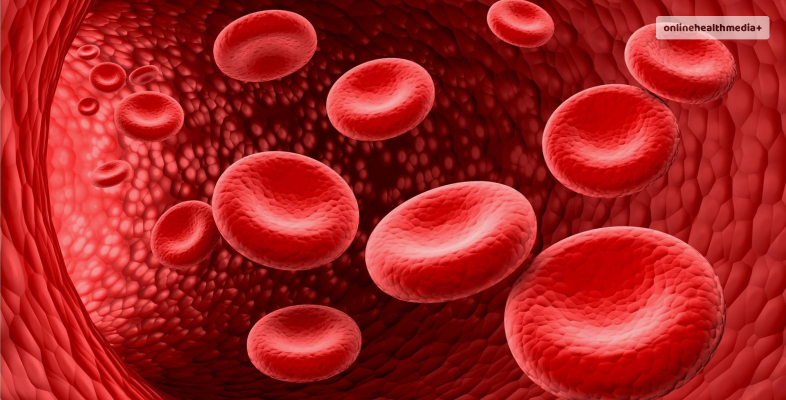
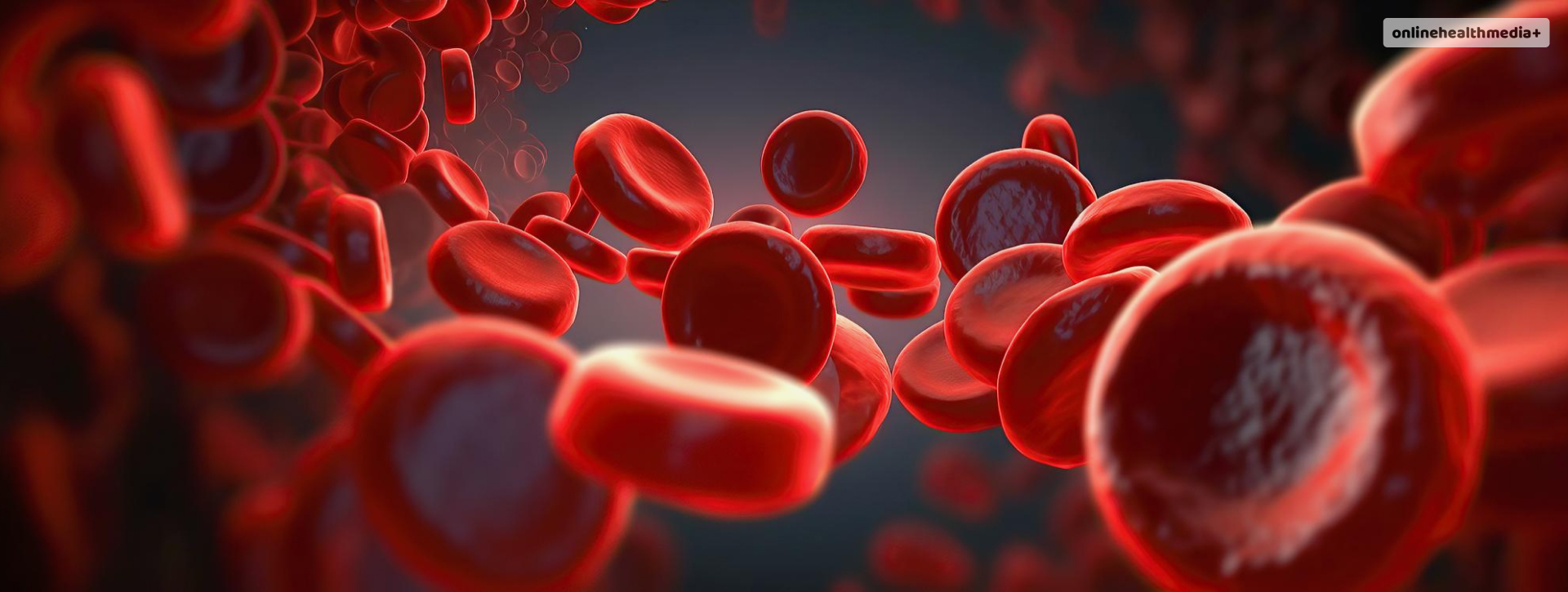
Sickle cell disease is due to mutations in the gene encoding the beta-globin subunit of hemoglobin. It is a protein responsible for carrying oxygen from the lungs to the body’s tissues.
The normal hemoglobin protein consists of two alpha-globin and two beta-globin subunits, forming a complex known as hemoglobin A (HbA).
In individuals with sickle cell disease, there is a specific mutation in the beta-globin gene. This results in the production of abnormal hemoglobin molecules known as hemoglobin S (HbS).
What Type of Mutation Causes Sickle Cell Disease? Answered.
How does it happen? Let me take you back to elementary biology or life science class! Remember the first lesson your teacher would have given you on DNA and its building blocks? Well, to jog your memory, there are mainly four building blocks: Adenine, Thymine, Cytosine, and Guanine. Also represented as A, T, C, and G respectively.
So, in the case of sickle cell disease, a single base replacement takes place. The mutation responsible for sickle cell disease is a single nucleotide substitution in the beta-globin gene, leading to a change in the amino acid sequence of the hemoglobin protein.
This is also known as single base-pair point mutation. Specifically, a thymine (T) base is replaced by an adenine (A) base at the sixth position of the beta-globin gene’s coding sequence.
Consequently, this substitution results in the replacement of a glutamic acid residue with a valine residue at the sixth position of the beta-globin protein chain.
For those unaware, valine and glutamic acid are types of amino acids that are building blocks of proteins.
Underlying Mechanism
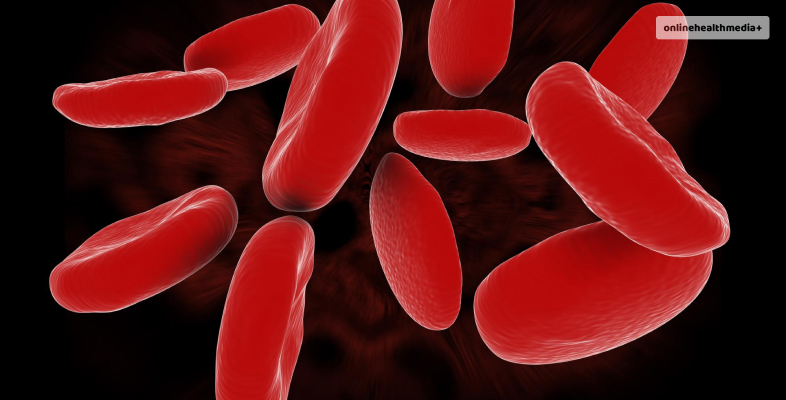
Moreover, the substitution of valine for glutamic acid alters the structure and function of the hemoglobin molecule. This leads to the formation of abnormal, elongated red blood cells known as sickle cells.
Unlike normal cells, which are flexible and disc-shaped, sickle cells are rigid and crescent-shaped. Additionally, this makes them prone to clumping together and obstructing blood flow in the small blood vessels.
Sickle cells in the bloodstream can lead to various complications, including.
1. Vaso-Occlusive Crises: Sickle cells can become lodged in the small blood vessels, causing episodes of severe pain known as vaso-occlusive crises. These painful episodes can occur unpredictably and may require hospitalization for pain management and supportive care.
2. Organ Damage: Chronic obstruction of blood flow by sickle cells can lead to damage to various organs and tissues, including the lungs, kidneys, liver, spleen, and bones. Over time, repeated vaso-occlusive crises and ischemic injury can contribute to organ dysfunction and failure.
3. Increased Infection Risk: Sickle cell disease impairs the immune system’s ability to fight off infections, leaving individuals susceptible to bacterial infections, particularly those caused by encapsulated bacteria such as Streptococcus pneumoniae. Infections can be life-threatening, especially in young children and individuals with compromised immune function.
4. Anemia: The presence of sickle cells in the bloodstream can lead to hemolytic anemia, a condition characterized by the premature destruction of red blood cells. In addition, anemia can cause fatigue, weakness, and pale skin due to decreased oxygen delivery to the body’s tissues.
Impact on Individuals and Communities
Sickle cell disease profoundly impacts the lives of affected individuals and their families. As well as on healthcare systems and communities.
The chronic nature of the disease, along with its associated complications and healthcare needs, can place a significant burden on individuals with SCD and their caregivers.
Managing sickle cell disease’s physical, emotional, and financial challenges requires a multidisciplinary approach involving healthcare providers, social support services, and community resources.
In addition to its impact on individual health and well-being, sickle cell disease poses significant societal challenges.
Additionally, limited access to healthcare services, inadequate resources for disease management and prevention, and stigma surrounding the condition can contribute to disparities in healthcare outcomes.
Consequently, affecting the quality of life for individuals with SCD, particularly those from marginalized or underserved communities.
Advancements in Treatment and Research
While there is currently no cure for sickle cell disease, there are significant advancements in the management and treatment of the condition.
Sickle cell disease life expectancy is usually lower than those without any condition. Thus, therapies aimed at reducing symptoms, preventing complications, and improving the quality of life for individuals with SCD include:
1. Hydroxyurea: Hydroxyurea is a medication that can help increase the production of fetal hemoglobin, a type of hemoglobin that is less prone to sickling. Hydroxyurea therapy has been shown to reduce the frequency of vaso-occlusive crises, hospitalizations, and the need for blood transfusions in individuals with SCD.
2. Blood Transfusions: Red blood cell transfusions may be used to manage severe anemia and prevent complications such as stroke in sickle cell patients. However, frequent transfusions can lead to iron overload and other potential risks, necessitating careful monitoring and management.
3. Bone Marrow Transplantation: For select individuals with severe sickle cell disease, bone marrow or stem cell transplantation may offer a potential cure by replacing diseased bone marrow with healthy donor cells. However, transplantation carries significant risks and is typically reserved for individuals with severe diseases who have suitable donor matches.
4. Gene Therapy: Emerging gene therapy approaches aim to correct the underlying genetic mutation responsible for sickle cell disease by introducing normal copies of the beta-globin gene into stem cells. While still in the experimental stages, gene therapy holds promise as a potential curative treatment for SCD.
Conclusion – what type of mutation causes sickle cell disease
Sickle cell disease is a complex genetic disorder characterized by the presence of abnormal hemoglobin molecules in red blood cells, leading to various complications and health challenges.
The underlying genetic mutation responsible for SCD produces abnormal hemoglobin S molecules, which can cause red blood cells to become rigid and sickle-shaped, leading to vaso-occlusive crises, organ damage, anemia, and increased infection risk.
Despite the significant impact of sickle cell disease on individuals and communities, advancements in treatment and research offer hope for improved outcomes and quality of life for individuals affected by this condition.
By raising awareness, promoting research, and advocating for improved access to healthcare services and resources, we can work towards better understanding, management, and, ultimately, a cure for sickle cell disease.
Know more about the causes of sickle cell disease? Let us know in the comments below.
Also read
- Tips Every Aspiring Nurse Should Know.
- 5 Tips to Take Care of Your Sensitive Skin.
- Can You Take Too Many Vitamins? Understanding The Risks And Benefits.